Tummy Tuck Recovery Kits
Sort by
Complete Recovery Supplies
Includes wound care, incision protection, and comfort items to make healing easier.
Tummy Tuck Recovery: Timeline, Tips, And What To Expect
You've done the hard part, choosing your surgeon and scheduling your abdominoplasty. Now comes the question every patient has: what does tummy tuck recovery actually feel like, and how long until you're "back to normal"? The short answer: recovery is a series of predictable phases with milestones you can plan for. The long answer, the one that helps you heal better and avoid setbacks, is below.
This guide walks you through each stage of tummy tuck recovery, from the first 72 hours to the six‑month mark, with clear timelines, practical tips, and red flags you shouldn't ignore. You'll learn how to set up your home, control pain and swelling, protect your results, and know when to call your surgeon. If you want a smoother, safer recovery and long-lasting results, start here.
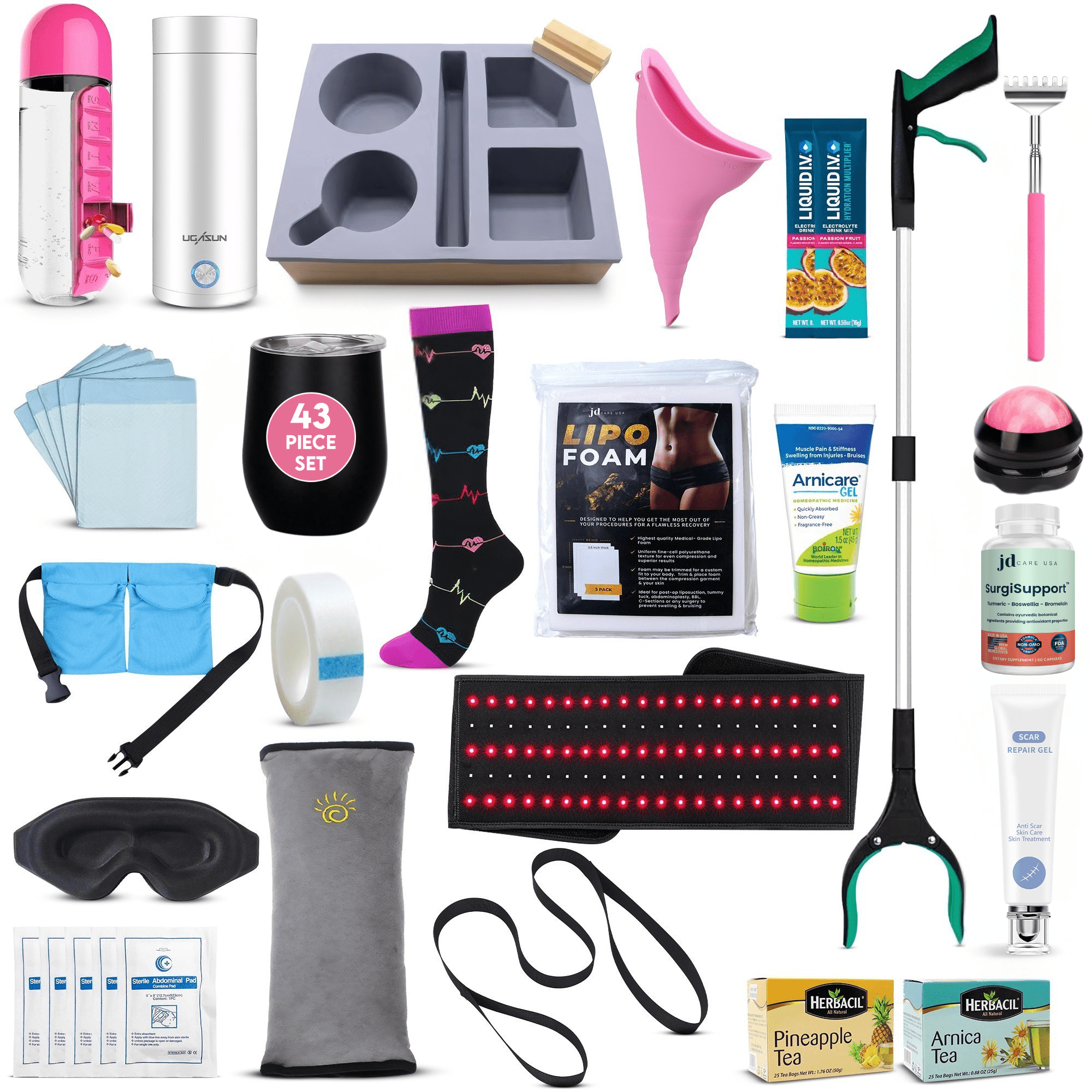
JD Care Tummy Tuck Recovery Kits
Tummy Tuck Kit (32pc) – Essential Recovery Basics in One Box
The Tummy Tuck Kit (32pc) is designed for people who want all the must-have basics ready to go without overbuying. It’s ideal if you’re still planning your tummy tuck, have your surgery date booked, or are already home and realizing how many small items you actually need. This kit focuses on core recovery essentials: absorbent underpads and ABD pads to protect your bed and incision, gentle medical tape and dressings, a capsule water bottle with built-in pill organizer to keep hydration and medications on track, a leg lifter strap to help you get in and out of bed without straining your core, a female urinal and urine bags for bathroom trips when standing or walking is difficult, and a self-massage roller and drain-holder for more comfortable, organized recovery. It’s a practical, surgeon-curated bundle that covers the everyday realities of tummy tuck recovery and saves you from last-minute shopping.
Ultimate Tummy Tuck Kit (47pc) – Advanced Comfort, Scar Care & Independence
The Ultimate Tummy Tuck Kit (47pc) is a more comprehensive option for people who want maximum comfort and support—especially if you’re having a full tummy tuck, mommy makeover, or combining your abdominoplasty with other procedures. Along with the core items (underpads, ABD pads, gauze, drain holder, medical tape, leg lifter, female urinal, pill-organizer water bottle), this kit adds advanced extras to support healing: a red-light therapy scar wrap to help improve scar appearance, three lipo foam pads to support contouring and reduce swelling, arnicare gel and scar repair gel, plus arnica and pineapple recovery teas for a natural boost. You also get daily-life helpers like a grabber tool, back scratcher, bed tray, seatbelt pillow, and more—so you can move, rest, and ride in the car with less strain. It’s the best choice if you want an “everything is covered” kit that supports scar care, swelling control, hygiene, and independence throughout your recovery.
Both kits are meant to complement (not replace) your surgeon’s instructions, making it easier to feel prepared and supported whether you’re still researching, counting down to surgery day, or already recovering at home.
Recovery At A Glance: What Changes And When
Most patients follow a similar arc after a full tummy tuck (with or without muscle repair). Your path may vary based on health, surgical technique, and how closely you follow instructions, but this is the general roadmap.
- First 72 hours: You're sore, tight, and moving slowly. You'll walk slightly bent at the waist, use your compression garment, and manage drains if placed. Pain and nausea are highest on day 1–2, then start easing.
- Week 1: Daily short walks, frequent rest, careful wound and drain care. Showering is often allowed 24–48 hours after surgery if your surgeon okays it. Many patients still nap during the day.
- Week 2: Energy improves. Some return to light desk work if off narcotics and able to sit/stand comfortably. Drains (if used) are often removed when output falls below about 25–30 mL per 24 hours per drain for two consecutive days.
- Weeks 3–4: Less tightness, but swelling comes and goes ("afternoon puffiness" is common). Light cardio resumes: still avoid core strain and heavy lifting.
- Week 6: Many activity restrictions lift with surgeon clearance. You may start gentle core reactivation, but full-intensity abdominal work waits until 8–12 weeks.
- Months 2–3: Swelling continues to settle: numbness slowly improves. Clothes fit better: posture feels more natural.
- Months 4–6: Scars are maturing (often pink to reddish), firmness softens, and your abdomen feels more like "you." Final contour generally declares by 6–12 months.
Your two jobs throughout tummy tuck recovery: protect the repair (especially if muscles were tightened) and support healing with movement, nutrition, and consistent follow-up.
Pre-Op Preparation For A Smoother Recovery
Set Up Your Home And Support System
Preparation reduces stress, complications, and last-minute scrambles.
- Sleeping space: Arrange a recliner or bed with multiple pillows so you can rest on your back with your upper body elevated and knees slightly bent. Some patients place a pillow under the knees and another behind the low back to reduce tension on the incision.
- Pathways and essentials: Clear tripping hazards. Keep water, snacks, tissues, lip balm, phone charger, thermometer, and medications within arm's reach.
- Bathroom setup: A handheld shower head, non-slip mat, and a shower chair help in the first week. Place incision-friendly towels and extra gauze nearby.
- Clothing: Front-opening, loose tops and high-waisted, soft pants make dressing easier. Avoid anything that rubs the incision line.
- Help at home: Plan for a responsible adult with you the first 24–48 hours. If you have kids or pets, pre-arrange help with lifting and walks for 1–2 weeks.
Medications, Supplements, And Smoking Cessation
- Fill prescriptions early: Pain medication, anti-nausea meds (like ondansetron), antibiotics (if prescribed), and stool softeners. Many surgeons use multimodal pain control (acetaminophen, sometimes an NSAID if appropriate, and nerve medication such as gabapentin). Follow your surgeon's protocol.
- Hold supplements that increase bleeding: Common culprits include fish oil/omega‑3s, vitamin E, ginkgo, garlic tablets, turmeric/curcumin, and some herbal blends. Typically stop 1–2 weeks pre-op, but follow your surgeon's exact instructions.
- Avoid alcohol 48–72 hours pre-op and for at least a week post-op to reduce bleeding and medication interactions.
- Nicotine cessation: Stop smoking/vaping and all nicotine products ideally 4–6 weeks before and after surgery. Nicotine decreases blood flow and oxygen to skin and can cause wound breakdown and poor scarring.
What To Bring And Do On Surgery Day
- Wear loose, front-opening clothes and slip-on shoes.
- Leave jewelry and valuables at home.
- Bring your compression garment if the team asked you to.
- Take only the medications your surgeon cleared for surgery morning with small sips of water.
- Confirm your ride and the adult who'll stay with you the first night.
First 72 Hours: Safety And Comfort Essentials
Pain Control, Nausea, And Drains
Expect tightness and soreness, especially if muscle repair (diastasis recti correction) was performed. Most patients do best with scheduled pain medication for the first few days, then taper.
- Take pain meds as directed and with food to avoid nausea.
- Use anti-nausea medication at the first hint of queasiness to stay hydrated and keep pain meds down.
- Cold therapy is usually avoided directly on the abdomen early on because of altered sensation: if your surgeon allows, use brief, wrapped cold packs away from the incision.
- Drains: If you have them, you'll empty and record output 2–3 times per day. Strip the tubing as instructed to prevent clots. Keep a simple log (date/time, mL per drain). Secure drains to clothing or a lanyard in the shower to avoid tugging.
Sleeping Position, Walking, And Breathing Exercises
- Sleep slightly bent at the hips and knees to reduce tension on the incision and muscle repair.
- Short, frequent walks start the day of surgery or the next morning to reduce blood clot risk and improve lung function. Think 3–5 minutes every few hours.
- Use incentive spirometry or deep-breathing exercises every 1–2 hours while awake for the first couple of days.
Red Flags That Require Immediate Contact
Call your surgeon urgently or seek emergency care for:
- Sudden, significantly increased pain on one side, a tense bulge, or a fluid "sloshing" sensation (possible seroma or hematoma)
- Fever over 101°F (38.3°C), chills, spreading redness, or pus-like drainage
- Calf pain or swelling, chest pain, shortness of breath, or coughing up blood (possible blood clot/PE, call emergency services)
- Persistent vomiting or inability to keep fluids down
- Darkening skin at the incision edges or new severe numbness/weakness in the legs
Week 1–2: Wound Care And Early Mobility
Incision And Drain Care, Showers, And Dressings
- Dressings: Your surgeon may use skin glue, paper tapes (Steri‑Strips), or external sutures. Unless instructed otherwise, keep the area clean and dry, and don't remove surgical tapes until they loosen on their own.
- Showering: Many protocols allow a gentle shower 24–48 hours after surgery. Let soapy water run over the area: don't scrub. Pat dry with a clean towel or use a cool hairdryer setting. Absolutely no soaking (baths, pools, hot tubs) for at least 4–6 weeks or until incisions are fully closed.
- Drains: Empty as taught, record outputs, and keep entry sites clean. Drains are often removed once output drops below roughly 25–30 mL per 24 hours for two consecutive days per drain, but follow your surgeon's threshold.
Compression Garments: Fit, Wear Time, And Care
- Wear time: Typically 24/7 (except for brief showers) for the first 4–6 weeks to control swelling and help skin adherence. Some surgeons taper use after week 6.
- Fit: The garment should be snug and supportive without causing pain, tingling, or deep marks. Avoid creases or rolling that can create pressure lines on healing tissue.
- Care: Wash and dry according to instructions. Having a second garment makes hygiene easier.
Bowel Care, Hydration, And Gentle Movement
- Prevent constipation: Start a stool softener (e.g., docusate) while on narcotics. Add a gentle osmotic laxative (like polyethylene glycol) if you haven't had a bowel movement by day 2–3. Don't strain.
- Eat to heal: Aim for 1.2–1.6 g of protein per kilogram of body weight daily, plenty of fiber, and colorful fruits/vegetables for vitamin C, zinc, and antioxidants. Stay hydrated, urine pale yellow is a simple target.
- Movement: Keep walking several times daily. Avoid lifting more than 10–15 pounds and any motion that strains your core (no sit-ups, twisting up from bed: roll to your side first).
Weeks 3–6: Activity, Work, And Exercise
Driving, Desk Work, And Lifting Limits
- Driving: You can usually drive once you're off narcotic pain meds, can twist/shoulder-check comfortably, and can brake firmly without hesitation. For many, that's around weeks 2–3, but only when you meet all criteria.
- Work: Many return to desk work around weeks 2–3 for short days at first. Jobs requiring standing, lifting, or bending often need 4–6+ weeks.
- Lifting: Keep the 10–15 pound limit until your surgeon clears you, typically around week 6. If muscle repair was extensive, restrictions may last longer.
Exercise Progression And Core Protection
- Weeks 3–4: Light, low-impact cardio such as walking, easy stationary cycling, or gentle incline treadmill. No jogging or HIIT yet.
- Weeks 4–6: Add light resistance for arms, back, and legs while avoiding valsalva (breath holding) and any movement that directly loads the abdomen. Use machines or bands that keep your torso stable.
- Core: Even after week 6, reintroduce core training gradually. Start with diaphragmatic breathing, pelvic tilts, and transverse abdominis activation under guidance. Planks, crunches, and heavy compound lifts usually wait until 8–12 weeks or later, with surgeon clearance.
Managing Swelling, Numbness, And Tightness
- Swelling fluctuates and often worsens as you increase activity. The lower abdomen and pubic area can look puffier at day's end, normal. Continue compression and elevate when resting.
- Numbness around the lower abdomen is common and can take months to improve as nerves regenerate.
- Tightness or "pulling" sensations are expected while tissues remodel. Gentle posture resets (stand tall, then relax), short walks, and light mobility drills help. Sharp pain or asymmetrical bulging warrants a call to your surgeon.
Months 2–6: Long-Term Healing, Scars, And Results
Scar Care, Massage, And Sun Protection
- Silicone therapy: Once incisions are fully closed (often ~2–3 weeks post-op, but confirm timing), apply silicone gel or wear silicone sheets daily for several months to improve scar quality.
- Massage: Some surgeons recommend gentle scar massage after 3–4 weeks to soften firmness and help mobility. Use light pressure with fragrance-free lotion unless told otherwise.
- Sun: Keep scars covered or use broad-spectrum SPF 30+ every day for a full year. UV exposure can darken scars permanently.
When Sensation Changes And Firmness Improve
- Nerve recovery is slow. Tingling, itchiness, or "zingers" are signs of returning sensation. Numb patches often shrink between months 3–12.
- The abdomen's "board-like" feeling softens as swelling resolves and tissues relax. If focal areas stay firm and raised, ask about lymphatic massage, some surgeons endorse a short course with a trained therapist.
Expectations For Final Contour And Symmetry
- By 3 months, you'll see most of the shape. By 6 months, swelling is largely gone. Subtle refinement and scar fading continue up to 12–18 months.
- Minor asymmetries are normal: your body isn't perfectly symmetric to begin with. If a small dog-ear or contour irregularity bothers you, revision discussions usually wait until scars mature (often after 6–12 months).
Factors That Shape Your Recovery Timeline
Health, BMI, And Medical Conditions
- Lower BMI, good cardiorespiratory fitness, and well-controlled conditions (like diabetes, hypertension, thyroid disease) shorten recovery windows and reduce risks.
- If you're anemic or have low protein status, address this pre-op. Optimize iron, vitamin D, and protein intake with your surgeon's guidance.
Surgical Technique And Muscle Repair
- Full tummy tuck vs. mini: A mini typically has a shorter recovery and fewer restrictions. A full abdominoplasty with muscle plication increases tightness and time to exercise.
- Liposuction add-ons: More lipo can increase bruising and swelling, slightly prolonging recovery.
- Drains vs. drainless techniques (progressive tension/barbed sutures): Drainless methods can reduce seroma risk and simplify care for some, but instructions still matter.
Lifestyle, Nutrition, And Sleep Quality
- Protein-forward eating, hydration, and limiting ultra-processed foods support collagen and immune function.
- Sleep 7–9 hours with consistent elevation the first couple of weeks. Poor sleep correlates with more pain and slower healing.
- Absolutely avoid nicotine for at least 4–6 weeks post-op (longer is better). It's the single biggest modifiable risk for wound problems.
Risks, Setbacks, And When To Call Your Surgeon
Seroma, Infection, And Wound Separation
- Seroma: Fluid accumulation presents as a squishy or sloshy area, often with increased swelling or a fluid wave. Small seromas may resolve: larger ones are often aspirated in the office. Continued compression and activity modification help.
- Infection: Watch for redness that spreads, warmth, fever >101°F, or foul drainage. Call promptly, early antibiotics can prevent worsening.
- Wound separation (dehiscence): Small openings can occur at points of tension. Keep clean, avoid stretching, and follow your surgeon's dressing plan. Large separations require immediate evaluation.
Blood Clots And DVT Prevention
- Risk is highest in the first 2 weeks. Preventive steps include early ambulation, calf pumps, compression devices in the hospital, compression stockings, hydration, and blood thinners if prescribed.
- Seek urgent care for calf pain/swelling, one-sided leg warmth, sudden chest pain, shortness of breath, or fainting.
Activity Adjustments And Follow-Up Care
- If swelling spikes or you notice pulling at the incision after an activity, back off 24–48 hours, elevate, and resume with smaller increments.
- Don't skip follow-ups. Bring your drain log and medication list. Ask when to start silicone, massage, and any lymphatic therapy.
- If you're unsure about a symptom, call. Early course corrections beat late fixes every time.
Maintaining Your Results For The Long Run
Weight Stability, Fitness, And Core Strength
- Keep your weight steady within a 5–10 pound range. Large fluctuations stretch skin and can blur your contour.
- Train consistently once cleared: full-body strength 2–3 days/week, low-impact cardio for heart health, and progressive core work that respects form and breathing. Think quality over load.
- Posture matters. Strong glutes, back muscles, and deep core (transverse abdominis) showcase your abdominal contour.
Pregnancy, Weight Changes, And Future Procedures
- If possible, complete childbearing before a tummy tuck. Pregnancy can re-separate muscles and stretch skin, partially reversing results.
- Significant weight gain or loss can alter outcomes. If changes occur, your surgeon can discuss non-surgical options (scar care, microneedling, lasers) or, selectively, minor revision after tissues mature.
- Keep up with scar protection for a full year, sun control is the cheapest "revision" you'll ever do.
Conclusion
A smooth tummy tuck recovery isn't luck: it's a plan. Set up your space, line up help, and follow your surgeon's instructions to the letter. In the first 72 hours, prioritize safety, pain control, short walks, proper positioning, and drain management. Over the next six weeks, steadily expand movement without loading your core, keep compression consistent, and watch for red flags. From months 2–6, refine scar care and return to fuller activity with patience.
The big picture: protect the repair early, fuel your body, sleep, and move a little more each week. Do that, and you'll stack the odds toward low complications, better scars, and a result that still looks great years from now.
Also Read:
- A Comprehensive Guide to Tummy Tuck Surgery
- A Comprehensive Guide to Minimizing Scarring After Cosmetic Surgery
- Weight Loss Teas: Facts, Myths, and Ingredients
Other Recovery Kits:
Surgery Recovery
Liposuction Recovery
BBL Recovery
Mastectomy Recovery
Tummy Tuck Recovery FAQs
What is the typical tummy tuck recovery timeline?
Most tummy tuck recovery follows phases: days 1–3 tight and sore with short walks; week 1 focused on wound care and rest; week 2 energy improves, some desk work resumes; weeks 3–4 light cardio; around week 6 many restrictions lift; months 2–6 swelling and scars settle, with final contour by 6–12 months.
When can I drive, return to work, and exercise after abdominoplasty?
Drive once off narcotics and you can brake and shoulder‑check comfortably—often weeks 2–3. Many return to light desk work around weeks 2–3; jobs with lifting/standing often need 4–6+ weeks. Start light cardio by weeks 3–4, add gentle strength by weeks 4–6, and delay direct core work until 8–12 weeks with clearance.
How long should I wear a compression garment after a tummy tuck?
Most surgeons recommend wearing compression 24/7 (except brief showers) for 4–6 weeks to control swelling and help skin adherence. It should be snug, not painful or numbness‑inducing. Some patients taper after week 6 per surgeon guidance. Having two garments helps with hygiene while maintaining consistent compression.
What red flags during tummy tuck recovery mean I should call my surgeon?
Seek urgent help for fever over 101°F, spreading redness, pus‑like drainage, sudden one‑sided pain or a tense bulge, a fluid “sloshing” sensation, persistent vomiting, darkening skin at incision edges, or calf pain, leg swelling, chest pain, or shortness of breath—possible blood clot or pulmonary embolism.
When is it safe to fly after a tummy tuck, and how can I reduce DVT risk?
Short flights are typically considered after 1–2 weeks if you’re walking well, hydrated, and cleared by your surgeon; longer flights often wait 3–4 weeks. Reduce DVT risk with frequent walk breaks, calf pumps, hydration, loose clothing, and compression stockings. Some patients may need prophylactic blood thinners—ask your surgeon.
How can I sleep comfortably—and when can I sleep on my side—during tummy tuck recovery?
Early on, sleep on your back with your torso elevated and knees bent to reduce tension on the repair. Many patients can transition to partial side sleeping after 2–3 weeks when swelling and tightness ease, using pillows for support. Always follow your surgeon’s timeline and comfort cues.
References
American Society of Plastic Surgeons (ASPS). n.d. Tummy tuck recovery. American Society of Plastic Surgeons, Arlington Heights, IL, USA.
Mayo Clinic. 2025. Tummy tuck (abdominoplasty). Mayo Clinic, Rochester, MN, USA.
Cleveland Clinic. n.d. Tummy tuck (abdominoplasty): surgery, recovery, risks & results. Cleveland Clinic, Cleveland, OH, USA.
StatPearls. 2023. Abdominoplasty. StatPearls Publishing, Treasure Island, FL, USA.
Staalesen, T. 2012. A systematic review of outcomes of abdominoplasty. Swedish Council on Health Technology Assessment, Stockholm, Sweden.
Vidal, P., Berner, J.E. & Rancati, A. 2017. Managing complications in abdominoplasty: a literature review. Aesthetic Plastic Surgery, 41(3), pp.575–585.
Chaker, S.C., Albano, N.J., Wan, D.C., Mardini, S. & Cooley, B.C. 2024. Complications and risks associated with the different types of abdominoplasties: an analysis of 55,956 patients. Aesthetic Surgery Journal, 44(9), pp.965–978.
Rao, G.S., et al. 2025. Systematic review and meta-analysis evaluating the surgical safety and complication profile of abdominoplasty. Aesthetic Surgery Journal, 45(1), pp.71–83.
Myszkowska, B., Toboła-Wróbel, K., Dąbrowska, D. & Dąbrowski, J. 2025. Complications following abdominoplasty in post-weight loss patients: a systematic review and meta-analysis. SAR Journal of Biomedicine, 7(5), pp.413–419.
Morales Jr, R., Mentz, H., Newall, G., Patronella, C. & Masters, O. 2013. Use of abdominal field block injections with liposomal bupivacaine to control postoperative pain after abdominoplasty. Aesthetic Surgery Journal, 33(8), pp.1148–1153.
Lim, B., Seth, I., Cevik, J., Cuomo, R. & Milone, M. 2024. Innovations in pain management for abdominoplasty patients: a systematic review. Journal of Personalized Medicine, 14(11), 1078.
Arkoubi, A.Y., et al. 2024. Effect of compression garments on post-abdominoplasty outcomes: a systematic review of the current evidence. JPRAS Open.
Kosloski, F.R., et al. 2024. Effect of compression garments on the ventilatory function after abdominoplasty. Aesthetic Surgery Journal.
Ossola, P., Segna, E., Perren, A., Cassina, T. & Banz, V. 2021. Evidence on postoperative abdominal binding: a systematic review. International Journal of Surgery, 88, 105–112.
Rothman, J.P., Gunnarsson, U. & Bisgaard, T. 2014. Abdominal binders may reduce pain and improve physical function after major abdominal surgery – a randomized controlled trial. Danish Medical Journal, 61(4), A4941.